Can The Menopause Cause Joint Pain?

Finding it hard to uncurl your legs and get up off the sofa as quickly as you used to? More of a struggle to get out of the car or bed? Or after long periods sitting still? Have you got sore knees, tight hips, achy fingers or back pain? Aching joints are one of the most common symptoms of the menopause – for many, the most noticeable, as this stage of life and as a natural part of the ageing process.
Beginning with perimenopause, which typically begins during the early the mid-40’s and can last from three to five years, menopause is considered to start when a woman has gone for 12 months without menstruating; the average age of menopause onset in the UK is about 51 years old.
Triggered by hormones that fluctuate and decrease, many parts of the body are affected as hormone levels, in particular oestrogen, decline. In addition to menopause joint pain, perimenopause and menopause signal an end to reproduction, and impacts the vaginal tract, urinary and nervous systems, heart, brain, skin and bones.
WHY MENOPAUSE CAUSES JOINT PAIN
While bones become more brittle with age, one of the first signs of menopause onset can be joint pain, affecting knees, shoulders, neck, elbows and even hands. Old joint injuries may begin to ache. And as time goes on you may start to notice that you feel more aches and pain in those areas than ever. While the precise cause-and-effect of menopause and joint pain hasn’t yet been identified, there’s evidence that inflammation could be behind much of it. Pain, swelling and joint inflammation is often a signal of osteoarthritis (OA), the wearing down of protective tissue between bones. Since OA disproportionately affects women in menopause, and age, it’s likely that this is because oestrogen, which helps to reduce inflammation, can’t do its job as it is declining. So as its levels fall, inflammation may increase, causing discomfort and menopause-related arthritis.
Oestrogen also regulates fluid levels throughout the body, so just as your skin is direr and less elastic, the tissue of your joints may be too. Another theory is that oestrogen reduces pain perception, so when levels decline you’re more sensitive to pain.
There are other contributory factors – beyond hormones, carrying excess weight, leading a sedentary lifestyle, dehydration, poor diet, smoking and stress can all trigger or worsen joint pain.

DOES JOINT PAIN FROM MENOPAUSE GO AWAY?
Unlike many signs of menopause, joint pain may not diminish when hormones level out after menopause. So no, it may not go away. However, there are many lifestyle changes that can help ease the pain and prevent it from getting worse.
On the list of changes to make to your lifestyle should be Hormone Replacement Therapy (HRT). This is far and away the most effective treatment for menopause joint pain, alongside other symptoms of menopause, and should be discussed and monitored with your doctor.
Additional lifestyle changes to support HRT and help prevent menopause joint pain include:
- Diet: eating plenty of anti-inflammatory foods. Some food tempers inflammation while others trigger it. For the right balance, eat more of these inflammation fighters: berries, broccoli, avocado, tomatoes, green leafy vegetables like spinach and kale, citrus fruits, cherries, fatty fish like salmon, olive oil, nuts, dark chocolate (in moderation), olive oil, green tea, turmeric, and ginger. And avoid foods that contribute to inflammation such as refined carbohydrates like white bread and cake, fried foods, red meat and processed meats, sugary beverages, and foods with trans fatty acids like margarine.
- Exercise: regular movement keeps joints lubricated so they flex and extend more easily and with less pain. Low-impact activities like yoga, walking, swimming and cycling are gentler on the joints than high-impact sports like running. Exercise will also help you keep tabs on your weight, because excess weight puts stress on your joints as you move, so losing even a few pounts (weight loss is tough during the menopause transition) can mean exponential relief for weight bearing joints like hips and knees. Workout out with weights in the gym can help too: strengthening the supporting muscles around a joint provides stability. When joints are stable, they function better, and you have less risk of damage or an injury.
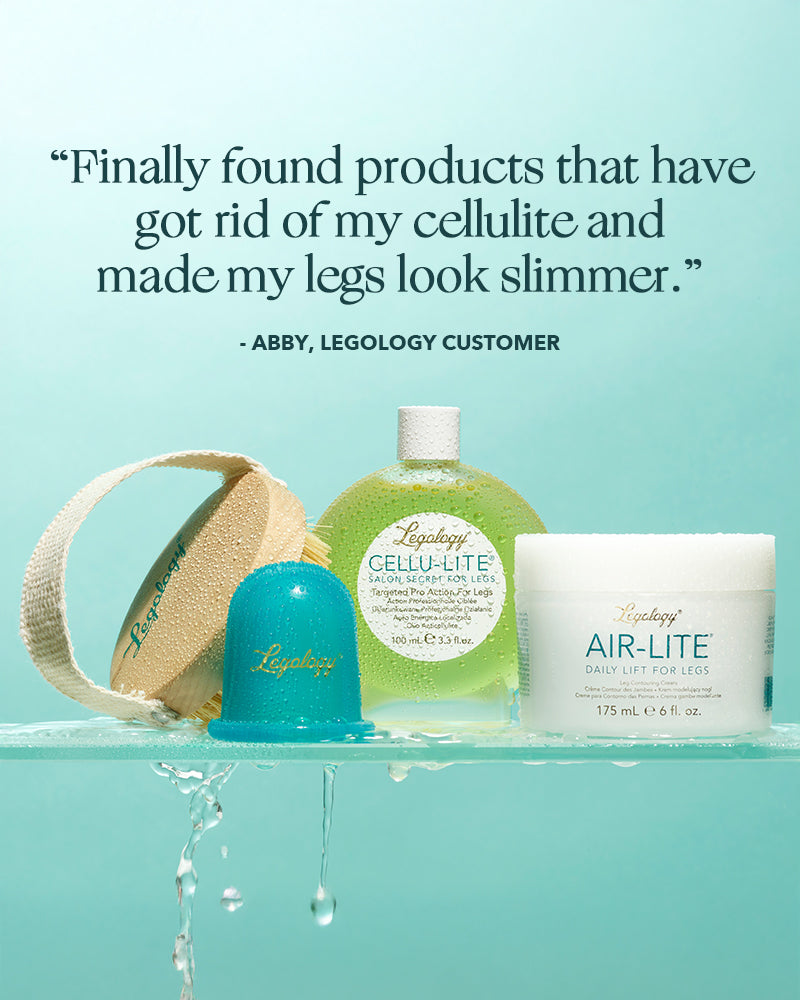
- Hydration: drink lots of water to keep tissues moist and supple and support the lymph in clearing away waste and hormones. Many women find that they suffer more with fluid retention during menopause, making their legs feel heavy and uncomfortable and aggravating cellulite. Legology Air-Lite cream was made to help shift the trapped fluid that gathers between fat cells and provide lightness, energy and comfort. Try to drink at least a litre of water – not a canned drink or coffee – daily, and add a few pieces of fruit, like cleansing lemon, for flavour.
- Stretch: too much sitting or computer time? At regular intervals, so every 20 or 30 minutes, stop what you’re doing and move. On a computer, stretch your forearms, do some wrist circles, or squeeze a soft ball. Get up from your desk and march in place and then stretch your legs and hips. The motion will keep your joints lubricated and minimise stiffness. Remember to strengthen your core too. Your body is one long chain of joints and muscles, and weakness at one part affects others. When the core muscles in your back, abdomen, hips, and buttocks are strong, it takes pressure off your knees and ankles.
- Destress: yes we probably sound like a broken record, but when it comes to joint pain, stress is especially problematic. It raises cortisol levels, and cortisol can cause additional inflammation in joints. Do what you can to keep stress in check. If stressed, consider taking a walk — in nature is best for a triple crown of stress- and joint-pain relief: nature, time away, and moderate exercise.
- Supplement: enhance your diet with menopause supporting supplements. Magnesium may help as it strengthens bones, maintains nerve and muscle function, regulates heart rhythm and blood sugar levels, and helps maintain joint cartilage. Other good options are glucosamine and chondroitin.